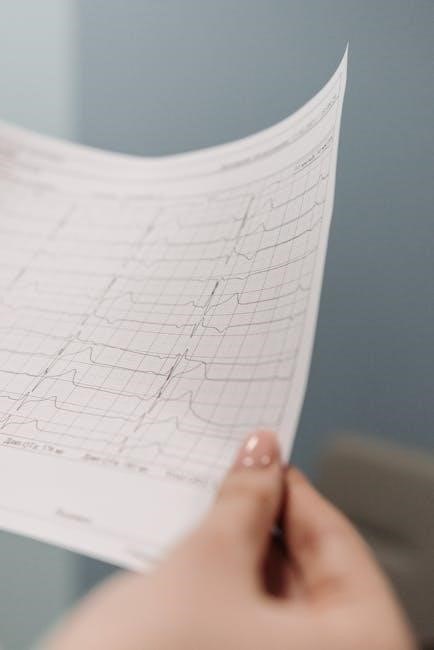
Rapid ECG interpretation is essential in emergency medicine, enabling quick diagnoses and timely interventions. It involves a systematic approach to analyzing heart rate, rhythm, and waveform morphology, ensuring accurate patient care.
Overview of ECG Importance
The electrocardiogram (ECG) is a cornerstone of cardiovascular diagnostics, providing critical insights into heart function and rhythm. It aids in detecting arrhythmias, ischemia, and structural abnormalities, guiding timely interventions. As a non-invasive tool, its rapid interpretation is vital for emergency medicine, enabling swift decision-making and improving patient outcomes. ECGs are essential for identifying life-threatening conditions and monitoring treatment effectiveness, making them indispensable in clinical practice.
Historical Context and Evolution
The ECG has a rich history, beginning with Willem Einthoven’s invention of the electrocardiogram in 1903. Over the decades, it evolved from cumbersome devices to portable, high-tech tools. The development of the 12-lead system and advancements in interpretation techniques have enhanced its diagnostic power. Modern ECGs integrate digital technology and AI, enabling rapid analysis and improving patient care. This evolution underscores its enduring importance in cardiology and emergency medicine.
Systematic Approach to ECG Interpretation
A systematic approach to ECG interpretation involves analyzing rate, rhythm, intervals, axis, and waveform morphology. This method enhances accuracy and enables timely, effective patient care decisions.
Step-by-Step Analysis of ECG Components
Step-by-step ECG analysis begins with assessing rate and rhythm, followed by evaluating intervals (PR, QT) and axis. Next, examine the P wave, QRS complex, and ST-T waves for abnormalities. This systematic approach ensures comprehensive evaluation, aiding in accurate diagnoses. Resources like Dubin’s methodology and online tutorials provide structured guidance for mastering this process efficiently.
Rate, Rhythm, Intervals, and Axis Assessment
Assessing heart rate ensures it’s within the normal range. Evaluating rhythm helps detect arrhythmias. Measuring intervals like PR and QT can reveal conduction issues. Determining the axis aids in identifying deviations in electrical activity. Using structured methodologies ensures accuracy and speed in ECG interpretation, vital in emergency settings for timely patient care.
QRS Complex and ST-T Wave Morphology
The QRS complex represents ventricular depolarization, while the ST segment and T wave reflect ventricular repolarization. Normal QRS duration is <1.12 seconds, with ST-T waves indicating repolarization. Abnormalities like ST elevation or depression signal ischemia, while T-wave inversion may indicate infarction. Bundle branch blocks alter QRS morphology. Accurate analysis of these patterns is critical for diagnosing cardiac conditions effectively.

Understanding ECG Leads
ECG leads provide a 360-degree view of the heart’s electrical activity. The 12-lead system includes chest and limb leads, each offering unique perspectives for accurate diagnosis.
12-Lead ECG System
The 12-lead ECG system is a standard tool for comprehensive cardiac assessment, combining limb and chest leads to capture the heart’s electrical activity from multiple angles. Limb leads (I, II, III, aVR, aVL, aVF) provide a frontal view, while chest leads (V1-V6) offer a horizontal perspective, enabling detection of ischemia, infarction, and arrhythmias. This system is essential for accurate diagnosis in clinical and emergency settings.
Chest Leads vs. Limb Leads
Chest leads (V1-V6) focus on the heart’s horizontal plane, capturing anterior and posterior activity, while limb leads (I, II, III, aVR, aVL, aVF) provide a frontal view. Chest leads are essential for detecting anterior wall ischemia, and limb leads help identify axis deviations and bundle branch blocks. Together, they offer a comprehensive view of cardiac electrical activity, aiding in accurate ECG interpretation.

Recognizing Common ECG Patterns
Identifying arrhythmias, ischemia, and infarction patterns is critical. Look for ST-segment elevation in MI, Q-waves in old infarcts, and P-wave absence in atrial fibrillation. Bundle branch blocks alter QRS morphology, guiding clinical decisions.
Arrhythmias and Their Identification
Arrhythmias are detected by analyzing R-R intervals and P-wave presence. Atrial fibrillation shows irregular rhythms without P-waves, while supraventricular tachycardia presents narrow QRS complexes. Ventricular arrhythmias, like PVCs or VT, display wide QRS patterns. Assessing rate, rhythm, and QRS morphology helps differentiate conditions, enabling timely interventions in acute care settings for improved patient outcomes.
Ischemia and Infarction Patterns
Ischemia and infarction patterns on ECG are crucial for diagnosing cardiac conditions. ST-segment elevation indicates myocardial infarction, while ST-segment depression suggests ischemia. Q-waves signify prior infarctions. T-wave inversion may indicate ischemia or ventricular hypertrophy. These patterns guide immediate treatment decisions, emphasizing the importance of rapid and accurate ECG interpretation in emergency settings to improve patient outcomes and reduce complications.
Bundle Branch Blocks and Other Abnormalities
Bundle branch blocks alter the ECG’s QRS complex, with left (LBBB) or right (RBBB) patterns indicating delayed conduction. LBBB shows wide QRS with notched R waves in lateral leads, while RBBB displays wide QRS with slurred R waves in V1-V2. Other abnormalities include hemiblocks and fascicular blocks, which require careful analysis to differentiate and guide appropriate clinical interventions for accurate diagnosis and management.

Case Studies for Practical Application
Real patient ECG examples provide hands-on learning, enabling practitioners to apply theoretical knowledge and refine diagnostic skills through practical, real-world scenarios and interpretation challenges.
Real Patient ECG Examples
Real patient ECG examples are invaluable for learning, offering practical insights into diverse cardiac conditions. These cases cover arrhythmias, bundle branch blocks, and ischemia, enabling clinicians to refine their diagnostic skills. A systematic approach is applied to each ECG, emphasizing rate, rhythm, and waveform analysis. Interactive tools and resources, such as PDF guides, further enhance understanding, making complex interpretations more accessible and accurate for both students and professionals alike.
Interpretation Challenges and Solutions
ECG interpretation presents challenges such as complex arrhythmias, subtle ischemia signs, and artifacts. Clinicians must overcome these by using systematic approaches, AI tools, and educational resources. Structured methodologies and interactive guides help refine skills, while AI assists in faster, more accurate analyses. Continuous learning and practice with real patient cases enhance proficiency, ensuring reliable and efficient ECG interpretation in clinical settings.

Role of AI in ECG Interpretation
AI accelerates ECG interpretation by analyzing patterns, detecting abnormalities, and providing instant insights, enhancing diagnostic accuracy and speed in clinical decision-making.
AI Tools for Faster Analysis
AI tools enhance ECG interpretation by quickly identifying patterns and abnormalities, reducing diagnostic time. They analyze waveform morphology, detect arrhythmias, and flag ischemia, improving accuracy. These tools integrate with clinical workflows, providing real-time insights and aiding in rapid decision-making. AI also supports educational purposes, helping learners master ECG interpretation through interactive platforms and automated feedback.
Future Trends in ECG Technology
Future trends in ECG technology include wearable devices for continuous monitoring, AI-driven predictive analytics, and real-time cloud-based interpretations. Advances in electrode design and smartphone-integrated ECGs are expanding accessibility. These innovations enable early detection of cardiac anomalies, improve remote patient monitoring, and streamline data sharing between healthcare providers, enhancing overall patient outcomes and clinical decision-making.

Best Practices for Learning ECG Interpretation
Mastering ECG interpretation requires a systematic approach, starting with basic rhythm identification and progressing to complex waveform analysis. Utilize interactive learning tools and practice with real patient examples to enhance proficiency and confidence in rapid interpretation.
Simplified Methodologies
A systematic approach to ECG interpretation involves assessing rate, rhythm, intervals, axis, and then evaluating QRS complexes and ST-T wave morphology. This structured method ensures accuracy and efficiency, emphasizing understanding over memorization. Utilizing visual aids and step-by-step guides enhances learning, making complex patterns more accessible for rapid and reliable interpretation in clinical settings.
Interactive Learning Formats
Interactive learning formats, such as real patient ECG examples and step-by-step guides, enhance comprehension and retention. Visual aids, including vivid color illustrations, simplify complex concepts. Practical exercises and quizzes allow learners to apply knowledge, fostering confidence in rapid interpretation. These engaging tools cater to diverse learning styles, ensuring mastery of ECG patterns and abnormalities in a dynamic and effective manner.

Clinical Applications of Rapid ECG Interpretation
Rapid ECG interpretation is vital in emergency medicine, enabling quick detection of arrhythmias, ischemia, and other cardiac conditions, guiding immediate interventions and improving patient outcomes significantly.
Emergency Medicine Use Cases
Rapid ECG interpretation is critical in emergency settings for identifying arrhythmias, myocardial infarctions, and other acute conditions. It enables quick decision-making, such as administering thrombolytics or pacing, ensuring timely interventions. The HEARTS approach—History, Examination, Rate, Rhythm, Axis, ST segment, and Pacing—guides emergency providers to interpret ECGs efficiently, improving diagnostic accuracy and patient outcomes in high-stakes situations.
This systematic method ensures clinicians can act swiftly, reducing delays in critical care.
Monitoring and Diagnostic Implications
Rapid ECG interpretation enhances continuous monitoring in critical care, enabling early detection of ischemia, arrhythmias, and cardiac deterioration. It provides actionable insights for diagnosing acute coronary syndromes, guiding therapy adjustments, and preventing complications. Timely interpretation improves patient safety, reduces treatment delays, and streamlines clinical decision-making in dynamic care settings.
This approach ensures precise and efficient monitoring, optimizing diagnostic accuracy and patient outcomes.

Resources for Further Learning
Key resources include downloadable PDF guides, online courses, and tutorials. Dale Dubin’s EKG book and Ninja Nerds’ website offer comprehensive learning. These tools aid in mastering rapid interpretation techniques.
Recommended PDF Guides

Dale Dubin’s “Practical Guide to ECG Interpretation” and MS Holm’s structured approach PDF are highly recommended. These guides offer simplified methodologies, interactive formats, and real patient examples for rapid comprehension. They emphasize understanding over memorization, making complex concepts accessible. Both are available for free download, providing invaluable resources for learners seeking to master ECG interpretation efficiently.
Online Courses and Tutorials
Online platforms like Ninja Nerds and Dr. Seheult’s lectures offer comprehensive ECG tutorials. These resources provide structured approaches, real patient examples, and interactive formats for rapid learning. They emphasize understanding over memorization, making complex concepts accessible. Emergency medicine-focused courses also highlight practical applications, ensuring healthcare professionals can quickly interpret ECGs with confidence and accuracy in clinical settings.
Mastery of rapid ECG interpretation is crucial for accurate diagnoses and timely interventions. By following a systematic approach and practicing with real examples, healthcare professionals can enhance their skills, ensuring better patient outcomes and saving lives through swift, informed decision-making.
Key Takeaways
- Mastering rapid ECG interpretation requires practice and a systematic approach to analyze rate, rhythm, and waveform morphology accurately.
- Utilizing AI tools can enhance speed and precision in ECG analysis, supporting timely clinical decisions.
- Focusing on understanding rather than memorization ensures long-term proficiency in interpreting complex ECG patterns.
- Incorporating real patient examples and interactive learning formats improves skill retention and practical application.
- Continuous learning and staying updated with advancements in ECG technology are essential for optimal patient care.
Encouragement for Continuous Learning
Continuous learning is vital for mastering rapid ECG interpretation. Engage with online courses, tutorials, and interactive resources to refine your skills. Practice regularly with real patient examples to enhance accuracy and confidence. Stay updated on advancements in ECG technology and AI tools to deliver optimal patient care. Embrace lifelong learning to excel in this critical medical skill.